Unveiling the Truth About Sex
Ready to separate fact from fiction in the bedroom? This listicle tackles 7 widespread sex myths and facts, providing you with the accurate information you need for a healthier and more fulfilling sex life. Understanding these concepts is crucial for better communication, informed decisions, and ultimately, more satisfying intimate experiences. We’ll cover everything from heart attack risks and STIs to penis size and sexual satisfaction, debunking common misconceptions about sex in 2025. Let’s dive in and uncover the truth about sex myths and facts.
1. Myth: Sex Can Cause a Heart Attack
The idea that sex can trigger a heart attack is a pervasive myth, often fueled by dramatic portrayals in movies and sensationalized news stories. Many people, particularly those with existing heart conditions, worry about the strain sexual activity might place on their cardiovascular system. The truth is, for most individuals, even those with stable heart disease, sex is a relatively low-risk activity. While sexual activity does temporarily elevate heart rate and blood pressure, the exertion level is comparable to moderate physical activities like climbing two flights of stairs or taking a brisk walk. This is equivalent to approximately 3-5 METs (metabolic equivalents) of energy expenditure. Therefore, understanding the facts surrounding this common sex myth is crucial for maintaining a healthy and fulfilling sex life.

This myth deserves its place on a list of sex myths and facts because it addresses a serious concern that can negatively impact intimate relationships. Fear of a heart attack can lead to anxiety and avoidance of sex, affecting both physical and emotional intimacy. By dispelling this myth, we can empower individuals to enjoy a healthy sex life without undue worry.
Features of Sexual Activity in Relation to Cardiovascular Health:
- Moderate Cardiovascular Activity: The physical exertion during sex is generally mild to moderate.
- Temporary Increase in Heart Rate and Blood Pressure: These increases are normal physiological responses to physical activity and are usually transient.
- Low MET Level: The energy expenditure during sex is relatively low, further emphasizing its moderate intensity.
Pros of Sexual Activity for Cardiovascular Health:
- Stress Reduction: Sex is a known stress reliever, which can positively impact overall cardiovascular health.
- Safe for Most with Stable Heart Conditions: For the majority of people with managed heart disease, sexual activity is considered safe.
- Potential Cardiovascular Benefits: Regular sexual activity might contribute to improved cardiovascular health over time.
Cons and Cautions:
- Extremely Small Increased Risk Immediately Following Sex: There is a statistically small, but measurable, increase in risk immediately after sexual activity. However, this risk is minimal for most individuals.
- Consult a Doctor with Severe Heart Conditions: Individuals with severe, unstable, or uncontrolled heart conditions should consult their doctor before resuming sexual activity.
Examples and Supporting Evidence:
- A study published in JAMA (2011) found that sex triggered only about 1% of all heart attacks.
- The American Heart Association supports sexual activity for most patients with cardiovascular disease.
Actionable Tips for a Healthy and Safe Sex Life:
- Post-Heart Attack: Wait 3-4 weeks after a heart attack before resuming sexual activity, and only with your doctor’s approval.
- “Stair Test”: If you can comfortably climb two flights of stairs without experiencing chest pain, you are likely able to safely engage in sexual activity.
- Medication Adherence: Always take prescribed heart medications as directed.
This myth, often popularized by medical dramas and sensationalized news stories, needs to be debunked. Understanding the facts about sex and heart health can help men, especially those in relationships or wanting to understand their partner’s concerns, to approach intimacy with confidence and enjoyment, leading to healthier and more fulfilling relationships.
2. Fact: STIs Can Be Transmitted Through Oral Sex
It is a crucial fact, and unfortunately a common sex myth misconception, that sexually transmitted infections (STIs) can be transmitted through oral sex. Many people mistakenly believe that only vaginal or anal intercourse carries the risk of STI transmission. This is demonstrably false. STIs, including herpes, gonorrhea, syphilis, HPV, and in some cases HIV, can be passed from genitals to mouth or vice versa. The mucous membranes in the mouth are susceptible to many of the same pathogens that infect genital tissues, making oral sex a viable route of transmission.

The risk of transmission varies depending on the specific STI. While often lower than the risk associated with vaginal or anal sex, it is still significant and should not be ignored. Both giving and receiving oral sex carry risks. Understanding this fact is vital for anyone who is sexually active, especially men in relationships who want to understand their partner’s body and protect both their own health and their partner’s. This particular sex myth and fact deserves a prominent place on this list because of the widespread misunderstanding surrounding this issue.
Features of Oral STI Transmission:
- Varied Risk: Transmission risk differs depending on the specific STI.
- Bidirectional Transmission: Both giving and receiving oral sex pose risks.
- Significant, Though Often Lower Risk: Compared to vaginal/anal sex, the risk is generally lower but still substantial.
Pros of Understanding This Fact:
- Better Protection: Knowledge empowers individuals to take appropriate protective measures.
- Effective Barrier Methods: Using barrier methods like dental dams or condoms significantly reduces the risk of transmission.
- Early Detection: Regular STI testing can identify infections early, enabling prompt treatment and preventing further spread.
Cons of Misunderstanding This Fact:
- Lack of Awareness: Many remain unaware of the risks associated with oral sex.
- Overlooked Symptoms: Symptoms of orally-transmitted STIs, which can sometimes be subtle, might be overlooked or mistaken for other conditions.
- Lower Perceived Risk = Less Protection: The perception of lower risk often leads to less frequent use of protection during oral sex.
Examples of Oral STI Transmission:
- Cases of oropharyngeal gonorrhea (gonorrhea infection in the throat) have been on the rise in recent years.
- HPV transmitted through oral sex is linked to increasing rates of throat and mouth cancers.
- Herpes simplex virus type 1 (HSV-1, traditionally associated with oral herpes) and type 2 (HSV-2, traditionally associated with genital herpes) can both infect either location (mouth or genitals) through oral sex.
Tips for Safer Sex:
- Barrier Methods: Use dental dams or condoms during oral sex. Learn more about Fact: STIs Can Be Transmitted Through Oral Sex for practical tips on using these barriers effectively.
- Regular Testing: Get tested for STIs regularly, especially if you are sexually active with multiple partners.
- Avoid Contact with Sores: Avoid oral sex if either partner has visible sores, bleeding gums, or oral infections.
- Asymptomatic Infections: Remember that STIs can be present even without visible symptoms. Regular testing is crucial.
This critical information regarding oral sex and STIs has been popularized by public health campaigns from organizations like the CDC and WHO, as well as comprehensive sex education programs. Understanding these sex myths and facts is key to responsible sexual health.
3. Myth: The Withdrawal Method is Highly Effective Birth Control
The withdrawal method, also known as “pulling out” or coitus interruptus, involves withdrawing the penis from the vagina before ejaculation. It’s often mistakenly considered a reliable form of birth control. However, this method is far from foolproof. While it offers some protection against pregnancy compared to unprotected sex, it’s significantly less effective than most other contraceptive methods. The withdrawal method relies on perfect timing and immense self-control, two factors that are often difficult to maintain during sexual activity.
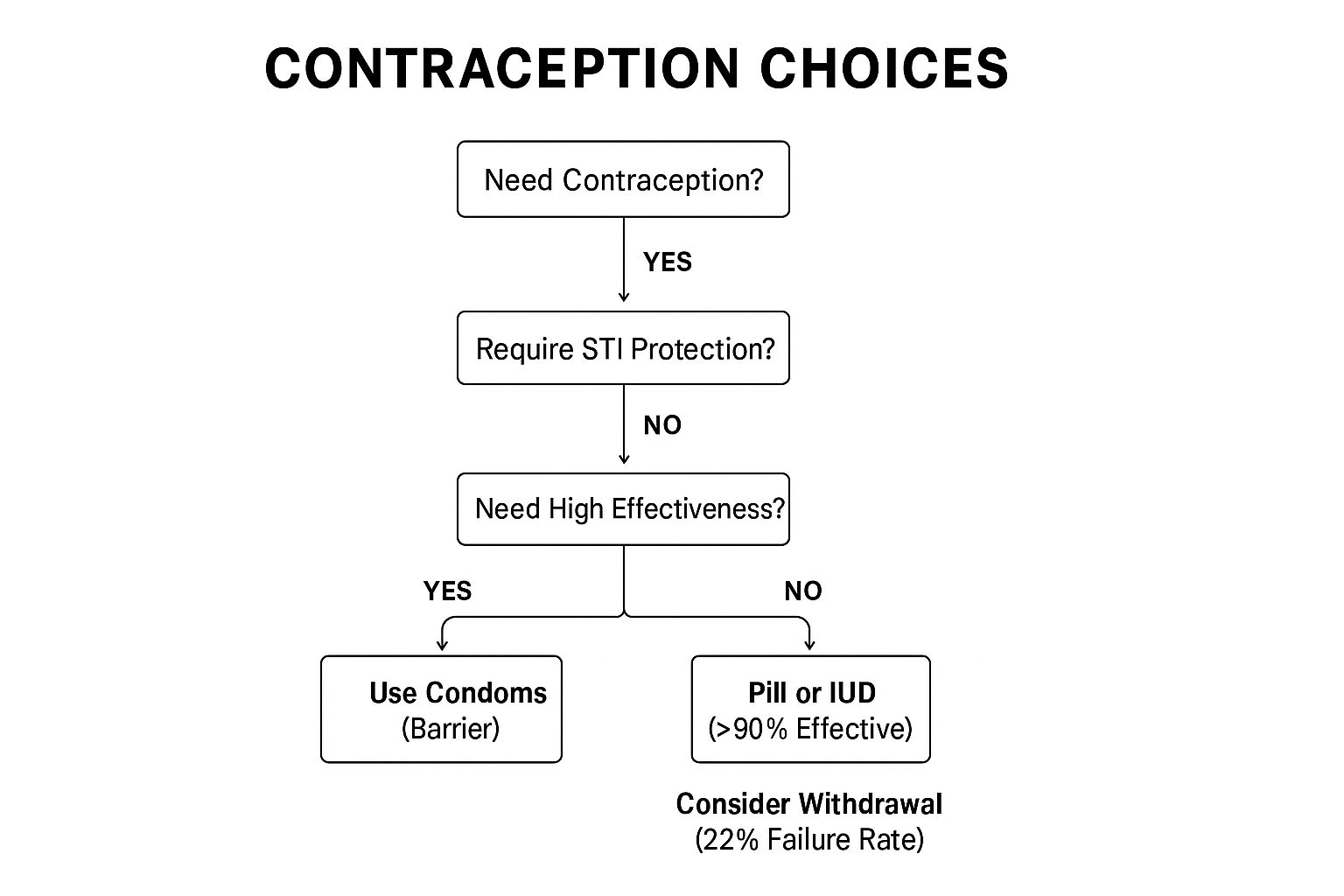
The infographic below presents a decision tree to help visualize the key considerations when deciding whether or not to use the withdrawal method.
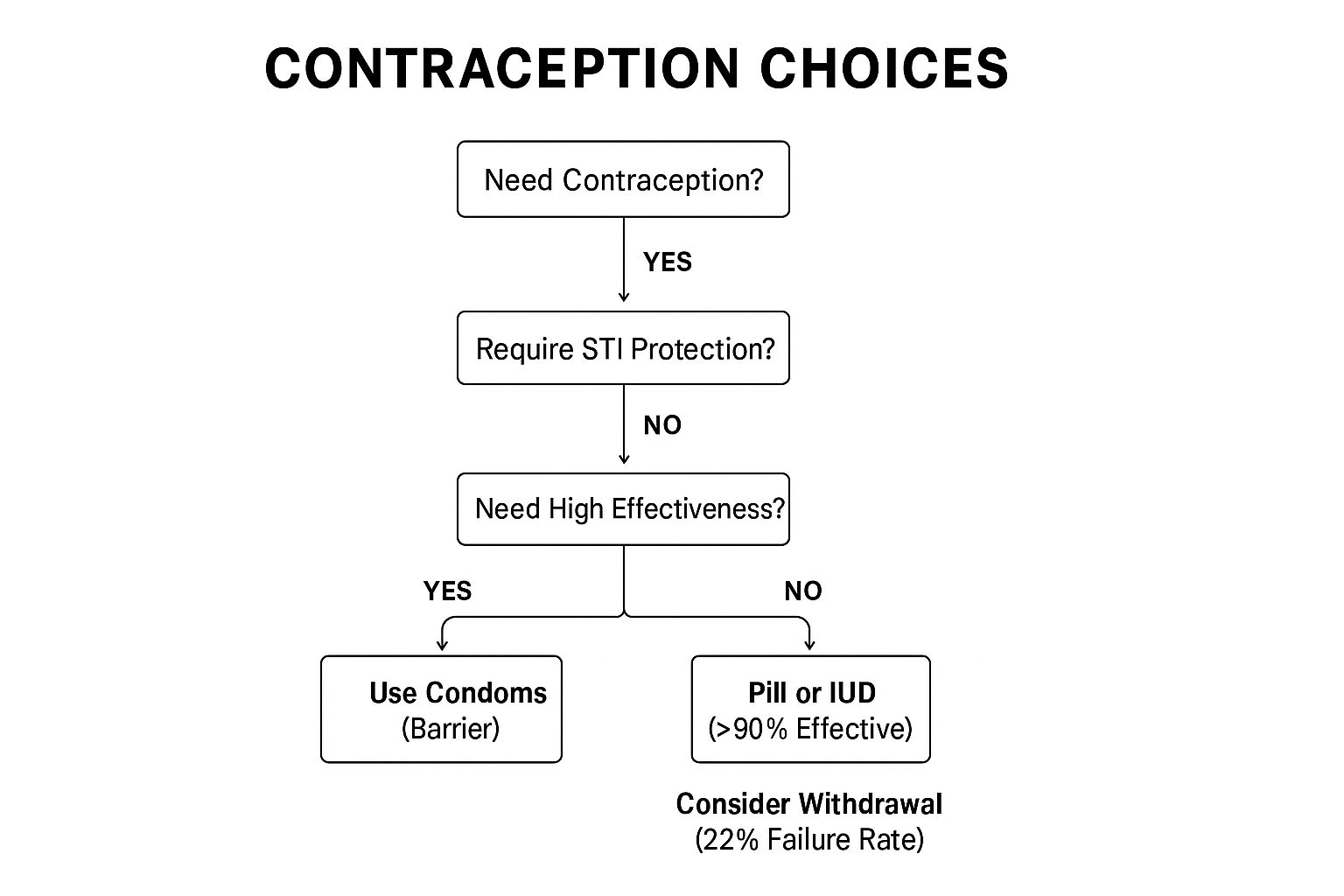
As the infographic demonstrates, even with perfect use, there’s still a risk of pregnancy, and with typical use, the failure rate is quite high. This highlights the importance of considering alternative methods.
With typical use, the withdrawal method has a failure rate of about 22% per year, meaning 22 out of 100 women using this method will become pregnant within a year. This high failure rate is attributed to several factors. First, pre-ejaculate, a fluid released before ejaculation, can contain sperm from previous ejaculations. Secondly, perfect timing is crucial, and even slight miscalculations can lead to unintended pregnancy. Finally, the withdrawal method requires significant self-control, which can be challenging to maintain during sexual arousal. This myth deserves a place on this list because its pervasiveness puts many individuals at risk of unplanned pregnancy.
Features of the Withdrawal Method:
- Requires precise timing and self-control
- Provides no protection against sexually transmitted infections (STIs)
- Pre-ejaculate fluid may contain sperm
- No financial cost or hormonal effects
Pros:
- Always available
- Requires no preparation, supplies, or prescriptions
- No side effects associated with hormonal birth control
- Can be used when other methods aren’t readily available
Cons:
- High failure rate (22% with typical use)
- Requires significant self-control
- Pre-ejaculate can contain sperm
- Provides no STI protection
- Can interrupt the sexual experience
Examples:
- Studies show pregnancy rates between 4-22% when using the withdrawal method, depending on perfect versus typical usage.
- Planned Parenthood statistics show it’s less effective than almost all other contraceptive methods.
Tips for Using the Withdrawal Method (with caution):
- Consider using withdrawal only as a backup to more reliable contraceptive methods.
- Urinating between ejaculations may help clear sperm from the urethra, but this isn’t foolproof.
- Combining withdrawal with fertility awareness methods (FAMs) can slightly improve effectiveness, but it still isn’t as reliable as other methods.
- For significantly better protection against pregnancy and STIs, use hormonal methods (pills, patches, rings, injections), intrauterine devices (IUDs), or barrier methods (condoms).
When and Why to Use This Approach (with strong caution):
Ideally, the withdrawal method should only be used as a last resort when no other contraceptive options are available. While it’s better than using no protection at all, the high risk of pregnancy makes it a less desirable choice. If you’re considering using withdrawal, have an open and honest conversation with your partner about the risks involved and the importance of consistent and correct use. Ultimately, prioritizing more effective methods ensures better protection against unplanned pregnancies and STIs. For men in relationships, understanding the limitations of the withdrawal method is crucial for shared responsibility in family planning and protecting your partner’s health. Remember, responsible sexual health requires informed decision-making and prioritizing effective contraception.
4. Fact: Sexual Orientation Is Not a Choice
One of the most pervasive and harmful sex myths is the idea that sexual orientation is a choice. This misconception contributes significantly to discrimination and negative mental health outcomes for LGBTQ+ individuals. The truth, supported by a wealth of scientific research, is that sexual orientation is not a choice but rather a fundamental aspect of human identity. This fact deserves its place in this list of sex myths and facts because understanding it is crucial for building a more inclusive and accepting society.
Sexual orientation emerges from a complex interplay of genetic, hormonal, neurological, and environmental influences. It refers to an enduring pattern of emotional, romantic, and/or sexual attractions to men, women, both, or neither. This isn’t a conscious decision but rather a deeply ingrained aspect of who a person is. For most people, sexual orientation emerges early in life and remains stable across the lifespan.
Features of Sexual Orientation:
- Emerges early in life: For many, initial awareness of their orientation begins in childhood or adolescence.
- Stable across the lifespan: While some individuals may experience shifts in their attractions or labels over time, fundamental orientation tends to remain consistent for most people.
- Exists on a spectrum: Sexuality isn’t binary. It’s more accurate to view orientation on a spectrum, with attractions varying in intensity and direction. Terms like bisexual, pansexual, and asexual reflect this diversity.
- Determined by multiple biological and environmental factors: While precise mechanisms are still being investigated, research points to a complex interplay of nature and nurture.
Pros of Understanding this Fact:
- Reduces stigma: Recognizing orientation as innate helps challenge prejudice and discrimination.
- Improves mental health: Acceptance of one’s sexual orientation, and acceptance from others, is correlated with significantly better mental health outcomes for LGBTQ+ individuals.
- Informs ethical healthcare: This scientific consensus guides healthcare professionals to provide appropriate and affirming care, rejecting harmful practices like “conversion therapy.”
Cons of Misunderstanding:
- Contested in some contexts: Despite scientific consensus, some religious and cultural beliefs continue to promote the false notion of choice.
- Contributes to discrimination: This misunderstanding fuels discriminatory practices and policies.
- Complex research: While research continues to uncover the biological mechanisms involved, the complexity of the subject makes it challenging to provide simple answers.
Examples of Scientific Evidence:
- Twin studies: Studies comparing identical and fraternal twins have shown higher concordance rates (i.e., both twins sharing the same sexual orientation) in identical twins, suggesting a strong genetic component.
- Neuroimaging studies: Research using neuroimaging techniques has revealed differences in brain structure and function between individuals of different sexual orientations.
- Cross-cultural studies: The consistent presence of non-heterosexual orientations across diverse cultures worldwide further supports the idea that it’s a natural variation of human sexuality, not a lifestyle choice.
Tips for Addressing Sexual Orientation:
- Focus on acceptance, not causation: When discussing orientation, prioritize acceptance and respect over trying to determine “why” someone is gay, straight, bisexual, etc.
- Support anti-discrimination policies: Advocate for policies that protect LGBTQ+ individuals from discrimination in employment, housing, healthcare, and other areas.
- Recognize questioning as normal: Understand that exploring one’s identity is a normal part of development, and questioning one’s orientation is common, especially during adolescence.
Popularized by:
The scientific consensus on sexual orientation has been affirmed by organizations like the American Psychological Association. Research by scientists such as Simon LeVay, Dean Hamer, and Lisa Diamond has contributed significantly to our understanding. Advocacy organizations like the Human Rights Campaign have also played a key role in promoting acceptance and fighting for LGBTQ+ rights. Understanding this fundamental aspect of human sexuality helps dismantle harmful sex myths and fosters a more inclusive and informed society.
5. Myth: Penis Size Determines Sexual Satisfaction
One of the most pervasive and damaging sex myths is the idea that penis size, specifically length, is the key to a partner’s sexual satisfaction. This myth, unfortunately, contributes to anxiety and insecurity in many men and distracts from the true elements of fulfilling sex. Scientific research consistently debunks this myth, highlighting that emotional connection, communication, skillful technique, attentiveness to a partner’s needs, and overall sexual compatibility are far more influential in determining sexual satisfaction than penis dimensions.

Globally, the average erect penis length falls between 5.1-5.5 inches (13-14 cm). It’s crucial to remember that the average vagina is only 3-4 inches (7.6-10.2 cm) in length when unaroused, and expands significantly during arousal. Furthermore, the majority of nerve endings in the vagina are concentrated in the outer third, a region easily accessible to any penis size. This biological reality underscores the fact that size is not the primary factor in stimulating the vagina. Learn more about Myth: Penis Size Determines Sexual Satisfaction
Pros of Understanding this Sex Myth and Fact:
- Reduced Anxiety and Improved Sexual Confidence: Dispelling this myth can alleviate performance anxiety and foster greater self-assurance in men.
- Focus on More Important Aspects: It shifts the focus towards crucial aspects of sexual intimacy like communication, foreplay, and mutual pleasure.
- Exploration of Diverse Techniques: Understanding this fact encourages exploration of various sexual techniques that prioritize pleasure beyond simple penetration.
Cons/Challenges:
- Persistent Media Messaging: The myth is continually perpetuated through media, particularly the pornography industry and advertisements for “enhancement” products.
- Body Image Issues: Societal pressures and unrealistic portrayals continue to fuel body image concerns related to genital size, impacting men’s confidence.
- Individual Preferences: While size isn’t the primary factor, individuals do have preferences, though these are diverse and often relate more to other qualities than just length.
Examples of Research Debunking the Myth:
- A 2006 study published in Urology revealed that 85% of women were satisfied with their partner’s penis size, while only 55% of men were satisfied with their own, demonstrating the disconnect between perception and reality.
- Research in the Journal of Sexual Medicine found no correlation between penis size and female sexual satisfaction.
- The concentration of nerve endings in the outer portion of the vagina further emphasizes that penetration depth, and therefore penis length, is less critical for pleasure than other factors.
Tips for Enhancing Sexual Satisfaction:
- Prioritize Communication: Openly discuss desires and preferences with your partner.
- Focus on Foreplay: Engage in extended foreplay to build arousal and enhance sensitivity.
- Master Diverse Techniques: Experiment with different positions, rhythms, and types of stimulation to discover what works best for both partners.
- Embrace the Multifaceted Nature of Sex: Remember that satisfying sex is a holistic experience encompassing physical, emotional, and psychological connection.
This myth deserves a prominent place in any discussion about sex myths and facts because it addresses a deeply ingrained insecurity affecting many men. Understanding the truth about penis size and sexual satisfaction can be truly liberating, leading to healthier relationships, greater confidence, and a more fulfilling sex life for both partners. This is especially valuable for men in relationships who want to understand their woman’s body and prioritize her pleasure. The myth is popularized by sources like the pornography industry’s selective casting, marketing for “enhancement” products, and cultural jokes and references in media. This perpetuates unrealistic expectations and reinforces anxieties surrounding penis size. By dismantling this harmful myth, we can pave the way for more open, honest, and pleasurable sexual experiences for everyone.
6. Fact: Sexual Dysfunction is Common and Often Treatable
This fact dispels a pervasive sex myth: that sexual dysfunction is rare, shameful, and untreatable. The reality is that sexual dysfunction is surprisingly common, affecting a significant portion of the population. Approximately 43% of women and 31% of men experience some form of sexual dysfunction at some point in their lives. This makes it a vital topic to address in any discussion about sex myths and facts, especially for men seeking to understand their own bodies and those of their partners. Understanding this reality can foster empathy, reduce stigma, and encourage those struggling to seek help.
Sexual dysfunction encompasses a wide range of conditions, impacting both men and women. These include, but aren’t limited to:
- Erectile dysfunction (ED): The inability to achieve or maintain an erection firm enough for satisfactory sexual intercourse.
- Premature ejaculation (PE): Ejaculation occurring sooner than desired, often before or shortly after penetration.
- Low desire (hypoactive sexual desire disorder): A persistent or recurrent lack of interest in sexual activity.
- Anorgasmia: Difficulty or inability to achieve orgasm, despite adequate sexual stimulation.
- Pain during sex (dyspareunia or vaginismus): Experiencing pain before, during, or after intercourse.
These conditions are legitimate medical concerns stemming from physical, psychological, or relationship-based causes, or a combination of factors. The prevalence of these issues increases with age but can affect individuals of all age groups. Furthermore, sexual dysfunction may be situational, occurring only in certain contexts, or generalized, impacting all sexual experiences. It can also be primary (lifelong) or secondary (acquired later in life).
Why This Matters:
Ignoring or dismissing sexual dysfunction can have far-reaching consequences, affecting not just sexual health but overall well-being and relationship satisfaction. Addressing the problem, however, often leads to significant improvements.
Pros of Seeking Treatment:
- High success rates: Many sexual dysfunctions respond well to treatment.
- Improved overall health: Addressing underlying health conditions contributing to sexual dysfunction, such as diabetes or heart disease, can benefit overall health. For instance, erectile dysfunction can sometimes be an early warning sign of cardiovascular issues. Early treatment for ED might also prevent future heart problems.
- Enhanced relationships: Successfully treating sexual dysfunction often improves intimacy, communication, and overall relationship satisfaction.
Cons and Challenges:
- Stigma: Unfortunately, significant stigma still surrounds sexual dysfunction, preventing many individuals from seeking professional help.
- Insurance coverage: Some treatments may not be fully covered by insurance, creating a financial barrier for some.
- Open communication: Effective treatment requires open and honest communication with healthcare providers, which can be challenging for some.
Examples of Successful Treatments:
- Vaginismus: This condition, characterized by involuntary vaginal muscle spasms, has an impressive 80-100% success rate with appropriate physical therapy.
- Combined approach: For many dysfunctions, a combination of cognitive-behavioral therapy (CBT) and medical treatment, such as medication or physical therapy, shows the highest success rates. Various therapies and treatments can help address sexual dysfunction. For some, exploring alternative methods like hypnosis for addiction can be beneficial in managing compulsive behaviors or anxieties related to sex. This approach can help individuals address the root causes of their anxieties and develop healthier coping mechanisms, ultimately contributing to a more fulfilling sex life.
- Erectile Dysfunction and Cardiovascular Health: Recognizing and treating erectile dysfunction can be crucial for overall health. As mentioned earlier, ED can be an indicator of underlying cardiovascular issues, and addressing it promptly may help prevent more serious heart problems down the line.
Tips for Addressing Sexual Dysfunction:
- Consult a specialist: Seek help from healthcare providers specifically trained in sexual medicine.
- Holistic approach: Consider both physical and psychological factors when exploring causes and treatments.
- Partner involvement: Include partners in the treatment process when appropriate, as it can significantly enhance communication and support.
- Address underlying conditions: Manage any underlying health conditions that may be contributing to the dysfunction, such as diabetes, heart disease, or depression.
The work of pioneers like Dr. William Masters and Virginia Johnson, along with the increasing acceptance fostered by figures like Dr. Ruth Westheimer, has helped normalize discussions about sexual problems. Pharmaceutical advancements, such as the development of Viagra, have also increased awareness and treatment options.
If you’re struggling with sexual dysfunction, remember that you’re not alone and effective treatments are available. Taking the first step towards seeking help can be transformative. Learn more about Fact: Sexual Dysfunction is Common and Often Treatable
7. Myth: Women Cannot Get Pregnant During Their Period
This pervasive sex myth falsely claims that women cannot get pregnant during their period. Understanding the truth about this misconception is crucial for responsible sexual health and family planning, especially for men in relationships who want to understand their partner’s body better. While the chances of conception are lower during menstruation, they are not zero. This myth’s persistence contributes to unplanned pregnancies and underscores the importance of accurate sex education. Therefore, it deserves a prominent place on this list of sex myths and facts.
Why This Myth is Dangerous
The belief that sex during menstruation is inherently safe perpetuates risky behavior and a misunderstanding of female reproductive biology. Men, in particular, should understand that relying on this myth can have significant consequences for their partners and any potential future family.
The Biology Behind the Myth (and the Facts)
Several factors contribute to the possibility of pregnancy during menstruation:
- Sperm Viability: Sperm can survive within the female reproductive tract for an impressive 3-5 days. If intercourse occurs towards the end of a woman’s period and she ovulates early in her next cycle, those resilient sperm could still be waiting to fertilize the newly released egg.
- Variable Cycle Lengths: Not all women have textbook 28-day cycles. Shorter cycles (e.g., 21 days) mean ovulation can occur much sooner, potentially overlapping with the end of menstruation. For example, a woman with a 21-day cycle might ovulate around day 7, while her period could last until day 5 or 6. This overlap creates a window for potential fertilization.
- Mid-Cycle Bleeding: Some women experience mid-cycle bleeding or spotting that can be mistaken for a period. If intercourse occurs during this time under the mistaken assumption of menstrual infertility, the risk of pregnancy significantly increases. This is especially pertinent for women using hormonal contraception, as breakthrough bleeding can mimic a period.
Pros of Understanding the Facts:
- More Effective Contraceptive Practices: Debunking this myth encourages consistent contraceptive use, regardless of the cycle phase.
- Holistic View of Fertility: It promotes understanding fertility as a continuum rather than distinct “fertile” and “infertile” days.
- Consistent Contraceptive Use: Knowing the facts encourages a proactive and responsible approach to family planning.
Cons of Believing the Myth:
- Increased Unintended Pregnancy Risk: The most significant downside is the potential for unplanned pregnancies.
- Difficulty Tracking Fertility: Complex and individual fertility patterns can be challenging to track accurately.
- Limited Applicability of General Rules: Individual variation in cycle length and ovulation timing makes general rules about menstrual safety unreliable.
Examples:
- Studies have documented pregnancies resulting from intercourse during reported menstruation.
- Breakthrough bleeding during hormonal contraceptive use has led to unintended pregnancies due to misinterpretation as a regular period.
Actionable Tips for Men and Their Partners:
- Use Contraception Consistently: The most reliable way to prevent pregnancy is to use contraception every time you have sex, irrespective of the woman’s cycle.
- Track Cycle Length: Encourage your partner to track her cycle length over several months to identify patterns and variations. Apps and calendars can be helpful tools.
- Acknowledge Irregularity: Understand that irregular cycles make fertility prediction less reliable.
- Factor in Lifestyle Influences: Be aware that stress, illness, and lifestyle factors can alter ovulation timing.
- Open Communication: Discuss family planning openly and honestly with your partner. Ensure you both understand the facts about fertility and contraception.
Popularized By:
This myth has been perpetuated through generations of misinformation, including:
- Folk Wisdom: Often passed down with good intentions but lacking scientific basis.
- Inaccurate Sex Education: Oversimplified or incomplete sexual education can leave gaps in understanding.
- Misunderstanding of Reproductive Biology: A general lack of knowledge about the complexities of the female reproductive system contributes to the myth’s persistence.
By understanding the facts and discarding this dangerous myth, both men and women can make more informed decisions about their sexual health and family planning. This knowledge is crucial for responsible and respectful relationships.
7 Key Sex Myths vs Facts Comparison
Topic   |
Implementation Complexity  |
Resource Requirements  |
Expected Outcomes   |
Ideal Use Cases  |
Key Advantages   |
|---|---|---|---|---|---|
| Myth: Sex Can Cause a Heart Attack | Low  (moderate physical exertion comparable to stairs) (moderate physical exertion comparable to stairs) |
Minimal (normal sexual activity) | Low risk for most; slight transient heart risk | Stable cardiovascular patients, general population | Stress reduction benefits; cardiovascular health improvement |
| Fact: STIs Can Be Transmitted Through Oral Sex | Moderate  (requires consistent barrier use) (requires consistent barrier use) |
Barrier methods (condoms, dental dams), testing | Prevents STI transmission; reduces infection spread | Sexually active individuals, especially with multiple partners | Increased awareness; effective prevention via barriers |
| Myth: The Withdrawal Method is Highly Effective Birth Control | Moderate  (requires timing, self-control) (requires timing, self-control) |
None (no supplies needed) | High failure rate (~22%); no STI protection | Backup contraception or when other methods unavailable | No side effects; always accessible |
| Fact: Sexual Orientation Is Not a Choice | Low  (innate, no action needed) (innate, no action needed) |
None | Recognition reduces stigma; acceptance improves well-being | Education, mental health support | Scientific consensus; supports ethical care |
| Myth: Penis Size Determines Sexual Satisfaction | Low  (behavioral understanding) (behavioral understanding) |
Education, communication skills | Improved sexual satisfaction by focusing beyond size | Sexual counseling, relationship enhancement | Reduces anxiety; promotes effective techniques |
| Fact: Sexual Dysfunction is Common and Often Treatable | Moderate  (requires medical/therapeutic intervention) (requires medical/therapeutic intervention) |
Healthcare providers, therapies, medications | High treatment success; improved quality of life | People experiencing sexual difficulties | Medical validation; relationship improvement |
| Myth: Women Cannot Get Pregnant During Their Period | Low  (educational effort needed) (educational effort needed) |
Contraceptive methods, cycle tracking | Awareness reduces unintended pregnancies | Contraceptive counseling, fertility awareness | Promotes consistent contraceptive use; fertility awareness |
Embrace the Facts for a Better Sex Life
Navigating the world of sex can be confusing with so many myths and misconceptions floating around. We’ve debunked some common sex myths and highlighted crucial facts – from understanding that STIs are transmitted through oral sex and that sexual orientation isn’t a choice, to recognizing that penis size isn’t the key to satisfaction and that sexual dysfunction is often treatable. Remember, the withdrawal method is not reliable birth control, and yes, pregnancy is possible even during a woman’s period. Separating fact from fiction regarding sex isn’t just about acquiring knowledge; it’s about empowering yourself to make healthier choices, fostering open communication with your partner, and ultimately, experiencing a more fulfilling and confident sex life. Mastering these sex myths and facts can significantly impact the quality of your intimate relationships and your overall well-being.
Understanding a woman’s body, including her pleasure zones, is a crucial part of a healthy and satisfying sex life. Want to deepen your understanding and enhance your intimacy? Explore the world of female pleasure and anatomy with G-Spot 101. Visit G-Spot 101 to unlock a wealth of knowledge and take your sexual understanding to the next level.
The post Uncover the Truth: Top Sex Myths and Facts Debunked appeared first on G Spot 101 .
Intimate Tickles found this article quite interested, and we thought you might to. We give all the credit for this article to gspot. Click Here To Read This Article From It's Original Source